State of California Benefits Identification Card Activation
You are eligible for Medi-Cal benefits because you have been approved for SSI/SSP benefits. The first month of your eligibility for Medi-Cal benefits is the month you applied for SSI/SSP, as long as you were eligible for SSI/SSP in that month.
BENEFITS IDENTIFICATION CARD
You have now received or will shortly receive a plastic Benefits Identification Card (BIC). This BIC is used to verify your eligibility for Medi-Cal benefits, allowing your Medi-Cal providers to bill for your medical and/or dental care. If your doctor or your health care provider tells you that your Medi-Cal eligibility is listed for a county in which you do not reside, you must contact your Social Security Administration (SSA) office to have them correct their records.
If you received Medi-Cal in the past, you may already have a plastic card that can be used again. If you lose your card, contact your local county of social services office and ask for a new card.
HOW TO PAY FOR PAST MEDICAL BILLS SINCE APPLYING FOR SSI/SSP
If you received Medi-Cal covered medical and/or dental services from a Medi-Cal provider since you applied and became eligible for SSI/SSP, that provider can bill Medi-Cal for those services. This may include a number of months before you receive your BIC. However, you must contact the Medi-Cal providers you saw during this period so that these providers can bill Medi-Cal. Payment for services over one year prior to receiving your BIC, requires a Letter of Authorization (Form MC180) showing the initial payment information. You can obtain this form by bringing your award letter or a letter from the SSA to your county social services office. You also should bring in copies of your medical and/or dental bills to assist in determining what month(s) you need to request Medi-Cal benefits.
The Medi-Cal program may be able to help pay for medical and/or dental expenses that you had in any of the three months before the date of your SSI/SSP application. To receive this help, you must be eligible for Medi-Cal in the month(s) Medi-Cal covered services were provided. You must make the request for Medi-Cal coverage for those months within a year of the month you had the medical and/or dental services. To make your request for coverage for those months, please contact your local county of social services office in your area. A list of county of social services offices is enclosed. Call the telephone number listed for your county. The county worker will help you locate the Medi-Cal office nearest your home.
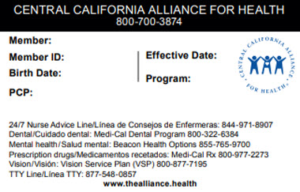
Below is an example of what your Alliance Member ID card will look like:
Where Can I Access My Medi-Cal Member Services?
You can access your member services online through your plan’s website and the Covered California website. Each service manages different aspects of your coverage. Also, your local county office will take care of specific parts of your Medi-Cal membership. Your health insurance company handles:
- Premium payments: When you need to make a premium payment, your health insurance company will accept it online or by phone.
- ID cards: Your insurance company will issue your membership ID card. They can also send you a replacement card if you lose it.
- Benefits and eligibility: Every insurance plan has unique benefits and eligibility requirements. A representative from your insurance company can explain these details to you.
- Claims: The insurance company can inform you how you paid your service claims when you need to verify this information.
- Covered medical providers: Your plan’s company can help you find a covered medical provider or change your primary care physician.
Meanwhile, Covered California takes care of:
- Enrollment: You can determine if you qualify for a special enrollment period, learn when you can enroll or enroll in a Medi-Cal plan through Covered California.
- Application information: Covered California handles changes to application information such as income verification, proof of residency and citizenship.
- Eligibility: When you request a quote from Covered California, they will determine if you or a family member has Medi-Cal eligibility.
- Coverage cancellation: If you want to cancel your Medi-Cal plan, you can request this cancellation through Covered California.
- Changing to a private plan: You can enroll in a private plan through Covered California if you will lose your Medi-Cal coverage soon.
When you need to renew your Medi-Cal plan, your county social services office will assist. They will get in contact with you if they need any information or send you a renewal form. For further assistance, you can contact your county’s Medi-Cal office or the Medi-Cal Member Helpline (1-800-541-5555).
How Do I Access Member Services?
Medi-Cal members can receive member services through the Internet or by phone. Most insurance plans have online member assistance, and many companies also allow you to call them to receive direct help. Covered California also has online member services that you can access through an account. You can make a Covered California account even if you already submitted an application through another method.
Where Can I Find My Card Number and Member Number?
After you enroll in Medi-Cal, you will get an enrollment package in the mail from your insurance company. This package will include a membership card and information about your health insurance account. Your welcome letter from the insurance company may also mention your membership ID number. If you want to make an online account for member services with your insurance plan, you need these numbers to create an account.
How Do I Pay My Premium Online?
Your health insurance company will receive all premium payments. After you enroll in a plan, you should receive a bill that includes online payment instructions. Most companies require you to make an online account and provide information about your payment card or bank account. You may also have the option to set up recurring payments that automatically withdraw money from the account or card you specify. Covered California has information about each plan’s payment options on their member information website.
Be the first to comment